
Cutting the Cost of Your Treatment
At Premier Physical Therapy Clinic I aim to keep our fees as low as possible, providing you with professional and effective care at the best

At Premier Physical Therapy Clinic I aim to keep our fees as low as possible, providing you with professional and effective care at the best
Muscle and joint pain can be debilitating. Common symptoms of this particular type of pain can involve twitching or burning of the muscles and achy,
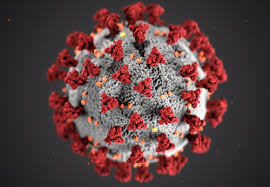
What are the symptoms of Coronavirus COVID-19? Symptoms can range from mild to severe illness. Some people will recover easily, and others may get very

The General Data Protection Regulation (GDPR) replaces the existing data protection framework under the EU Data Protection Directive. It is an EU Directive which enhances

Just two weeks of normal office life without exercise can put people on the path to diabetes, researchers have found Sitting at a desk all day,

This is a really interesting article form the Health and Living supplement of the Irish Independent: https://www.independent.ie/life/health-wellbeing/health-features/back-on-my-feet-why-ive-switched-to-a-standing-desk-36504065.html

I recently did a John Gibbons 2 day course in Dublin in May 2017; Spinal Manipulation and METs and the Vital Glutes and Psoas. John is

While back pain can be very painful and worrying, it is very common and rarely dangerous. A total of 84% of people worldwide will experience

Good Posture Helps Reduce Back Pain Correct posture is a simple but very important way to keep the many intricate structures in the back and

Ankle injuries are some of the most common for athletes competing in running, soccer, or basketball, but can plague even casual hikers and joggers. To